
Ari Cedars
@aricedars
Director of ACHD @Hopkinskids @Hopkinsheart, @HopkinsMedicine, proud father, aspiring wine snob. Opinions are my own, I share what’s interesting to me
ID: 3263814943
https://www.hopkinsmedicine.org/profiles/results/directory/profile/10005603/ari-cedars 01-07-2015 14:38:55
2,2K Tweet
2,2K Followers
392 Following

#arrhythmia is a plague in #CHD. A🇩🇰national system analysis shows arrhythmia (heart block, SSS, A and V arrhythmia)⬆️prevalence and ass with⬆️mortality. Likely anatomy should be ignored here(more TGA than TOF?) Alexandra Frogoudaki Alexander Vd Bruaene Alexander (Sasha) Opotowsky pubmed.ncbi.nlm.nih.gov/39233212/

RUBOTO, another failed pulmonary vasodilator trial in #Fontan. Perhaps we need to do a better job of identifying those who benefit and those who dont? Likely heterogeneous treatment effect. Alexander (Sasha) Opotowsky Alexander Vd Bruaene Swati Garekar pubmed.ncbi.nlm.nih.gov/39216715/

High PCWP ass with adverse outcomes in #TGA systemic RV. No surprise. The API data are surprising though. Excluding PCWP, all difference seems due to elevated systolic BP. No diff in HR, or CI. Need to think on this one! Alexandra Frogoudaki Shelby Kutty, MD, PhD, MHCM pubmed.ncbi.nlm.nih.gov/39206568/

#FALD remains a vexing condition. FONLIVER score (elastography + Plt ct) performs well but not that much better than VAST, and VAST has outcomes data (here severe fibrosis histology was outcome). I'm sure more data to come. Swati Garekar Alexander Vd Bruaene pubmed.ncbi.nlm.nih.gov/39260705/

Wow, such an important study! Exercise impact on liver in #Fontan. Upshot: exercise, even high intensity, appears safe! Only 10 patients but granularity of physiologic assessment impressive. DONT RESTRICT! Alexander Vd Bruaene Alexander (Sasha) Opotowsky Shelby Kutty, MD, PhD, MHCM pubmed.ncbi.nlm.nih.gov/37219588/

Johns Hopkins #ACHD team rocking it at the #ACHA Heart to Heart Regional Conference today 🤩🔥 Phenomenal sessions & workshops led by the greatest Drs. Ari Cedars Ari Cedars , Stacy Fisher Stacy Fisher, Konstantinos Aronis Konstantinos N. Aronis, MD PhD , Duke Cameron & Guillermo Torres-Viera!🫀👏🏻


I believe already reflected in the guidelines, but #BAV #aortopathy risk lower than #TAV, likely due to different pathophysiology. Truly important data to guide surgery! Shelby Kutty, MD, PhD, MHCM Swati Garekar Alexander Vd Bruaene Alexandra Frogoudaki pubmed.ncbi.nlm.nih.gov/37088130/

Data on #SCAI in #TOF, here in a younger population. SCAI3 still dominates, most common in those with more surgical stuff in the RVOT (RVOT patch, RV to PA conduit): Makes sense. Love the mechanistic approach! Swati Garekar Alexandra Frogoudaki Alexander Vd Bruaene pubmed.ncbi.nlm.nih.gov/39340504/

Very interesting data on #insulinresistance in #Fontan. The more we know➡️Fontan is a systemic illness with body-wide metabolic consequences! Fontan #metabolomics anyone? Kurt Schumacher Alexander (Sasha) Opotowsky Alexander Vd Bruaene Additional Ventures pubmed.ncbi.nlm.nih.gov/39375212/

Wow! Another important study on #Fontan related #Frailty. Could systemic metaboloic changes related to poor physical activity, physiologic, dietary and genetic factors be contributing to Fontan failure? Here 6MWD most impacted. Additional Ventures Kurt Schumacher pubmed.ncbi.nlm.nih.gov/39367114/

Excited to share our work looking at infective endocarditis in #ACHD! Despite more anatomically complex, lower IE mortality in ACHD vs. patients w/ structurally normal hearts. Thanks Stephen Dolgner and Keila Lopez MD, MPH 🫀 for your mentorship! Cardiology In The Young pubmed.ncbi.nlm.nih.gov/39385510/


Akbar et al showed ACHD candidates who were willing to consider HCV+ and DCD offers were more likely be transplanted and had similar post-transplant outcomes as recipients of HCV- and DBD organs. Armaan Akbar Ahmet Kilic Ari Cedars 🔗 jhltonline.org/article/S1053-…

Across 🇺🇸, 100 centers performed reoperations after #ASO in patients between 10-35yo: 1⃣ Most commonly AV, aortic root, coronary procedures 📶 Increase in procedures (esp. left-sided) 🫶 11% major complications; 2% discharge mortality The Annals of Thoracic Surgery: annalsthoracicsurgery.org/article/S0003-…

Interesting that the associations with #SCD in #Fontan are described markers of Fontan failure (PLE/Plastic bronchitis, ventricular dilation/dysfunction, NYHA). What's the mechanism? Alexander (Sasha) Opotowsky Alexander Vd Bruaene Shelby Kutty, MD, PhD, MHCM Swati Garekar pubmed.ncbi.nlm.nih.gov/39453360/

As if more confirmation was needed, #Fontan is a SYSTEMIC DISEASE. Information on total body health status may improve outcomes. Plasma biomarkers/metabolomics as possible indicators? Alexandra Frogoudaki Alexander (Sasha) Opotowsky Ali N Zaidi, MD Kurt Schumacher pubmed.ncbi.nlm.nih.gov/39423992/
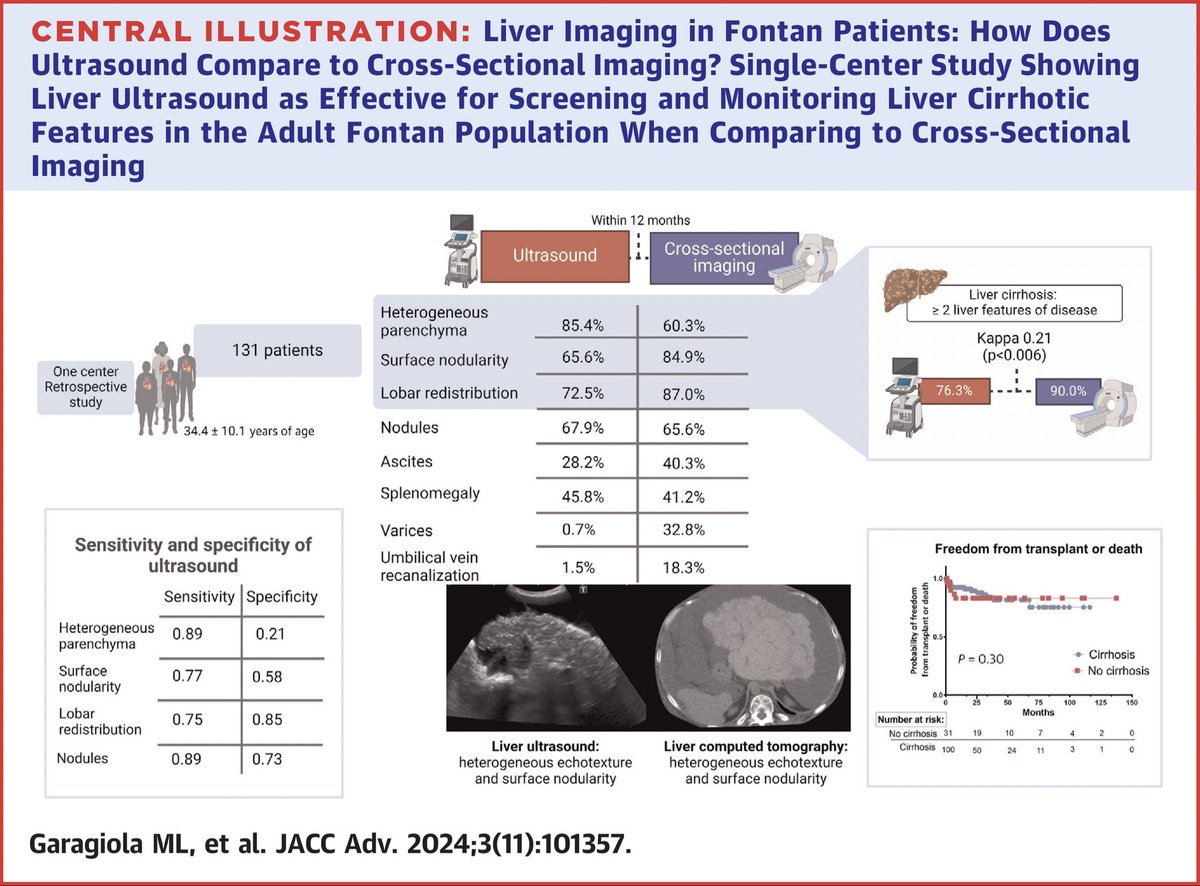
#ISACHD #TopPick Liver Imaging in Fontan Patients: How Does Ultrasound Compare to Cross-Sectional Imaging? jacc.org/doi/10.1016/j.… Rafa Alonso Candice Silversides Michael A. Gatzoulis Margarita Brida Oktay Tutarel, MD FESC Geetha Kandavello Blanche Cupido Ari Cedars Adrienne Kovacs, PhD Christopher DeZorzi

Interesting and important for counseling: #AVB and #LBBB more common after #SAVR in #BAV versus #TAV AND LBBB associated with adverse outcomes. Why not PPM? Doesn't that also cause LBBB? Alexander Vd Bruaene Alexandra Frogoudaki Elena gribaudo pubmed.ncbi.nlm.nih.gov/39440421/

