Neomi Shah
@neomishah
Physician Scientist | 🫁, Critical Care, 😴 Medicine | Sports Fan | Vegetarian | Not Afraid to Fail or Dream Big
ID: 2345766454
15-02-2014 23:03:09
6,6K Tweet
1,1K Followers
885 Following







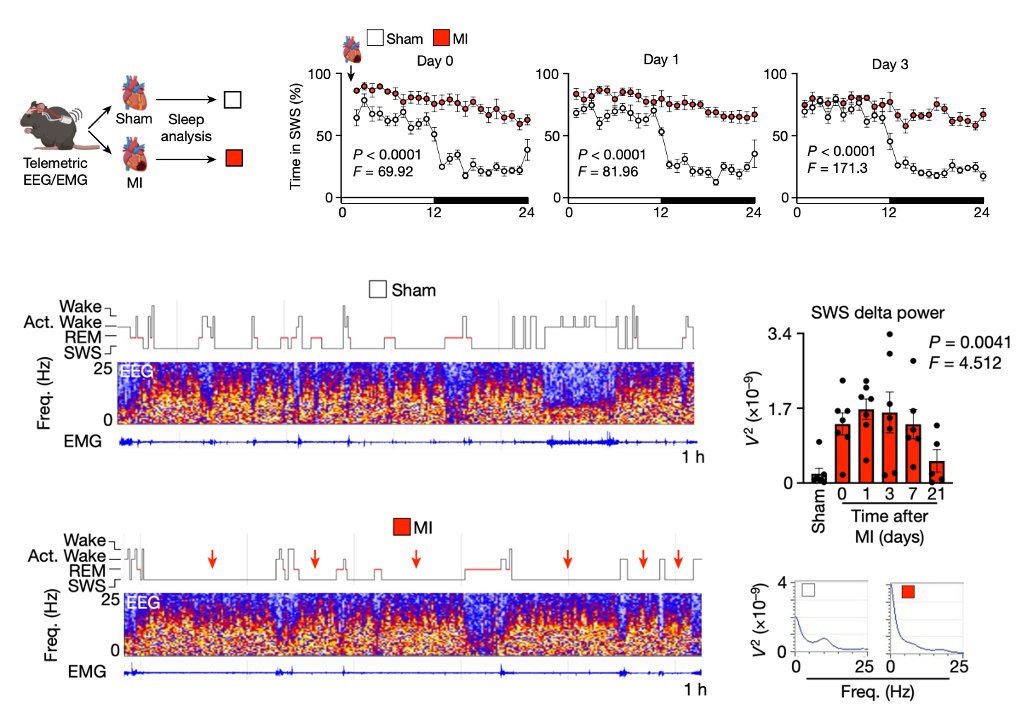
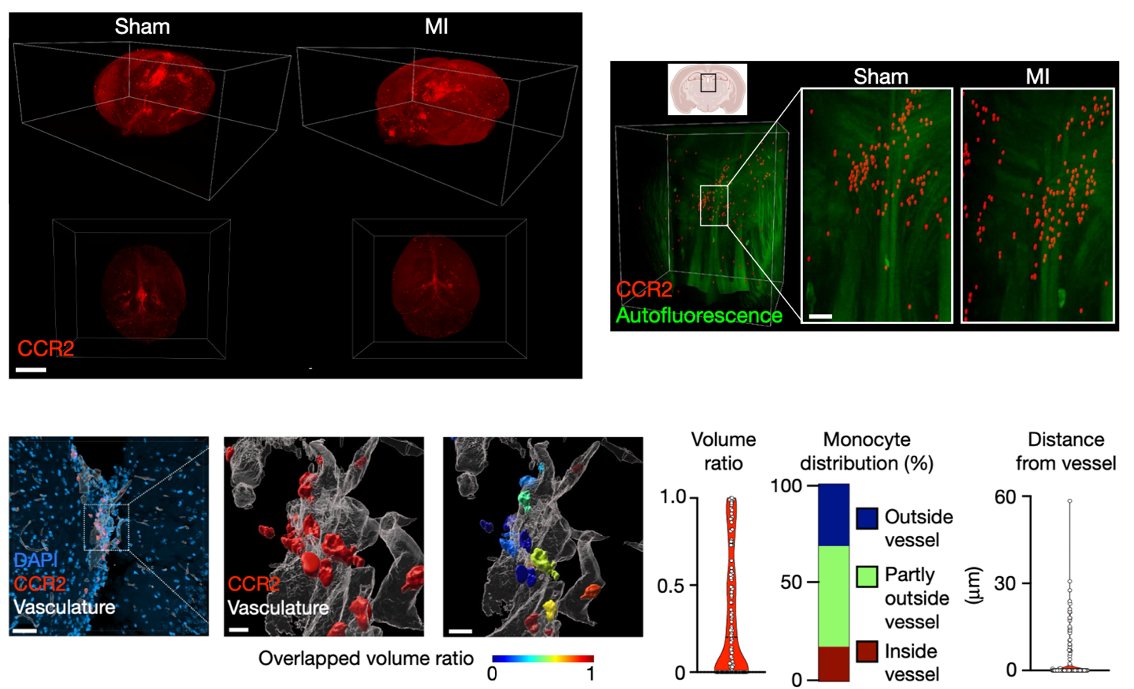
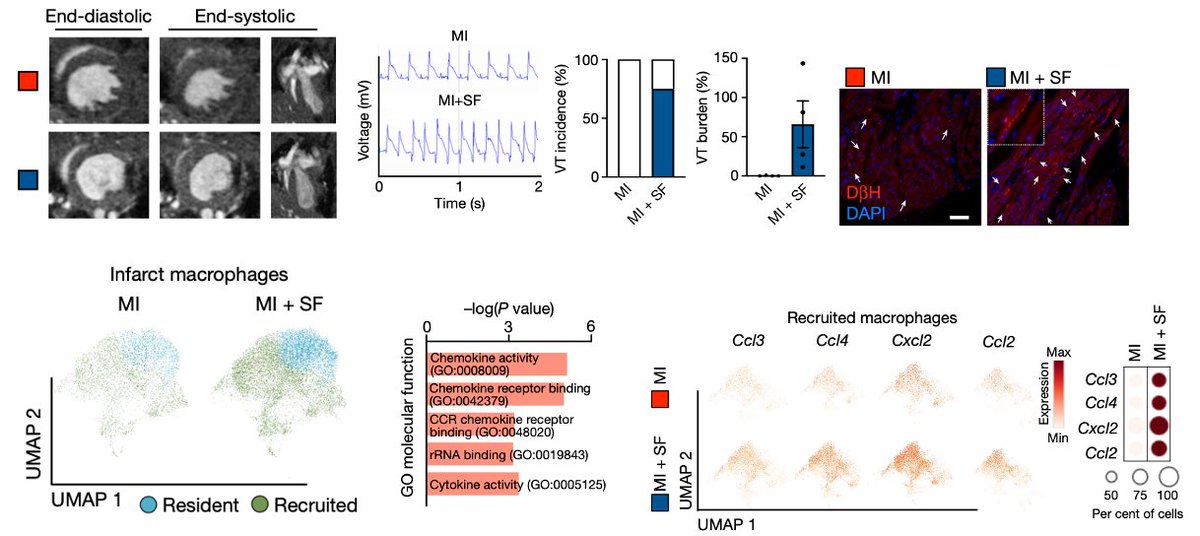
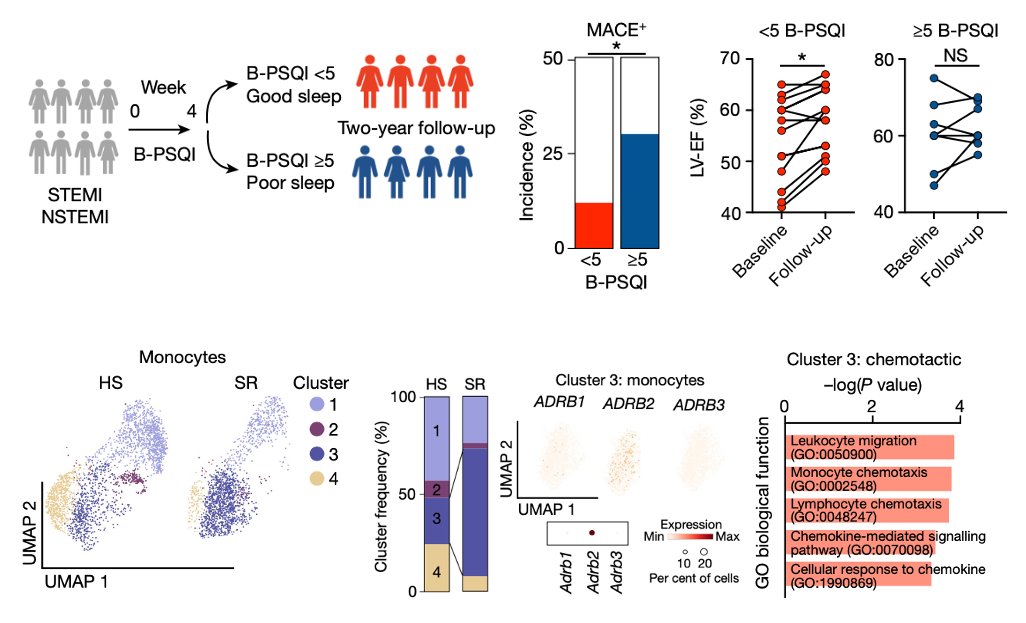
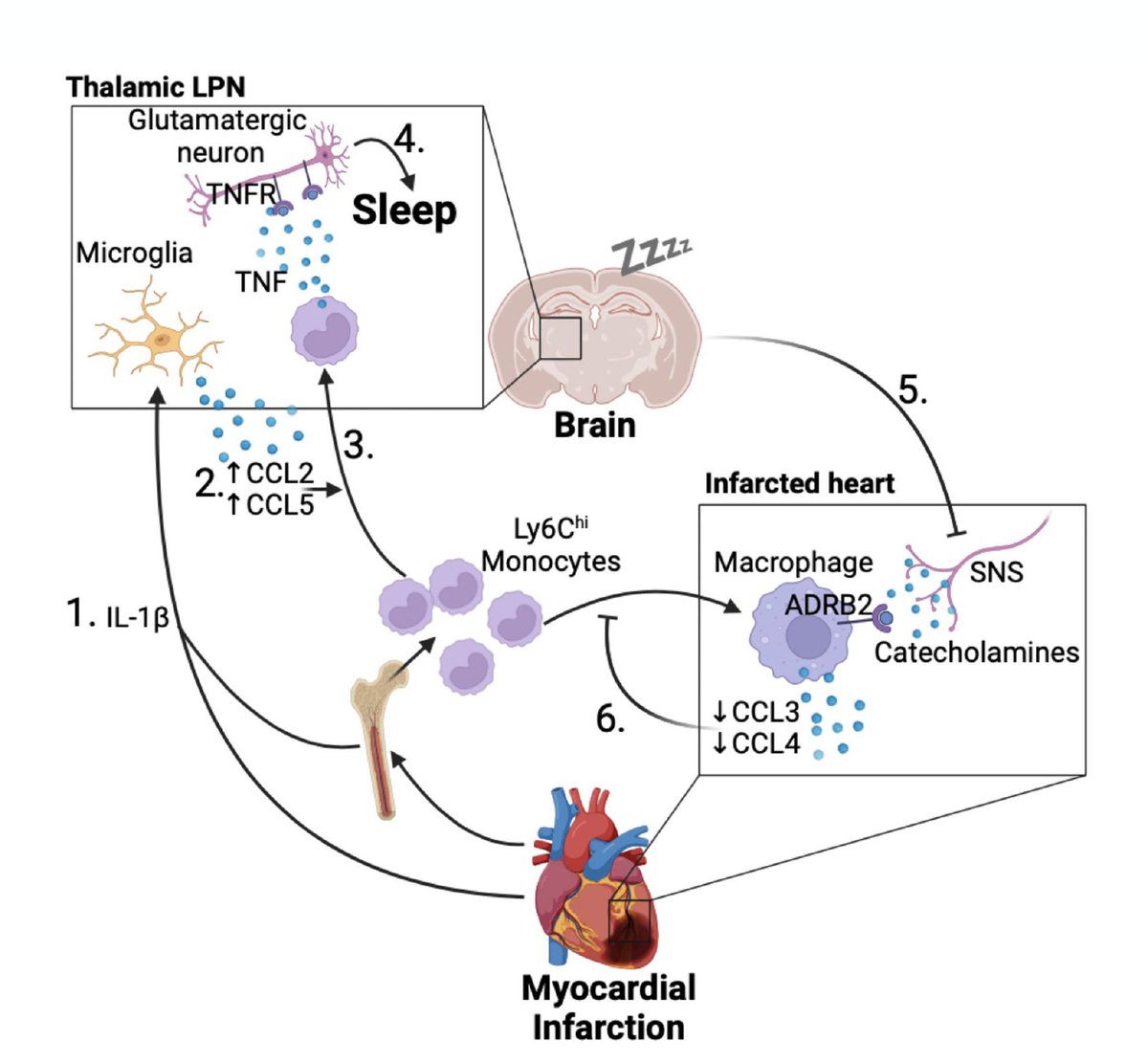
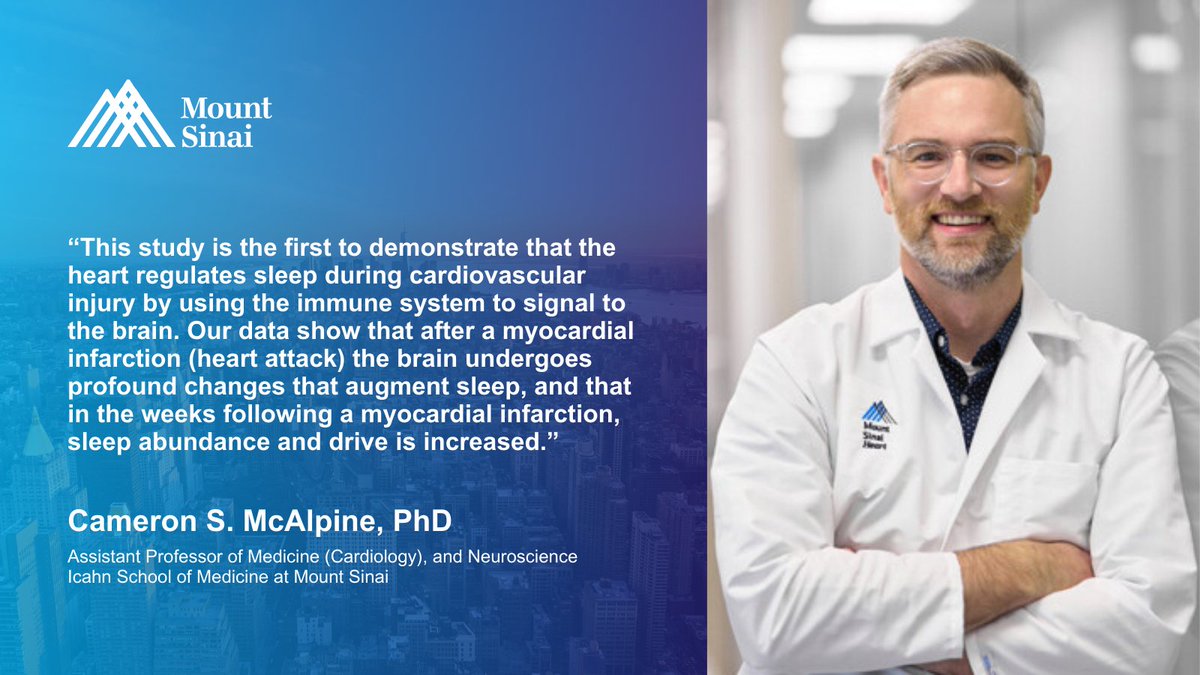
A new heart-brain-immune system discovery Following damage to the heart muscle from a heart attack, monocytes are recruited to the brain to promote sleep, limit inflammation, and healing. nature.com/articles/s4158… @peacemakerhuynh Cameron McAlpine Icahn School of Medicine at Mount Sinai Cardiovascular Research Institute at Sinai (CVRI)

STANTON!!!! 🔥🔥🔥 JUDGE!!!! 🔥🔥🔥🔥 JAZZ!!! 🔥🔥🔥🔥🔥 New York Yankees

Defense = JUDGE!! New York Yankees

Keep up hope New York Yankees fans

Send Blake back in the ninth Please We have some unfinished business New York Yankees

Send anyone in the ninth. New York Yankees are ready.

Proud to be a New York Yankees fan PERIOD

New Mount Sinai research reveals that a #HeartAttack can trigger a desire to get more #sleep, allowing the #heart to heal and reduce inflammation—and this happens because the heart sends special signals to the #brain. Learn more: mshs.co/3AmcAor Mount Sinai Department of Medicine

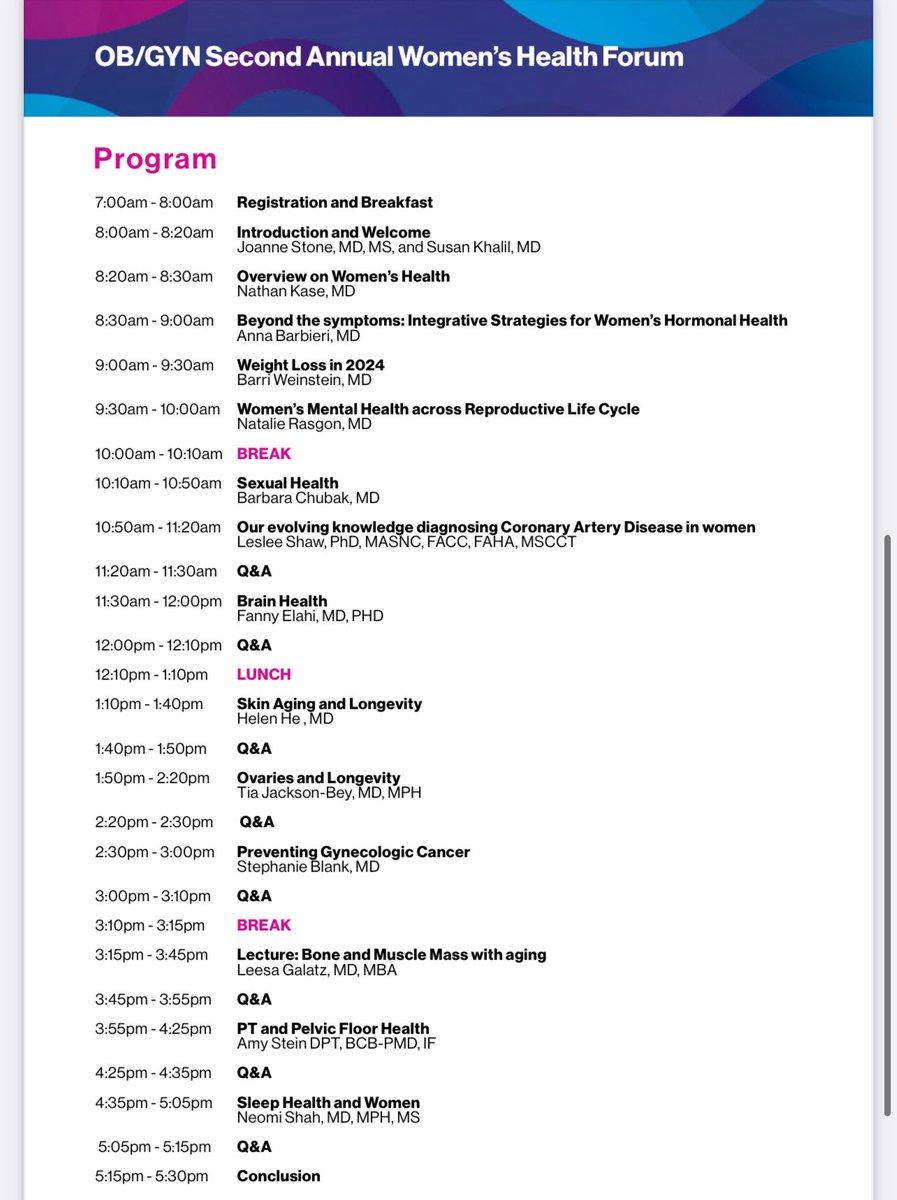
Excited to speak on Sleep and Women’s Health at the Icahn School of Medicine at Mount Sinai 2nd Annual OB/GYN Women’s Health Forum to expand knowledge, empower patients & connect with experts on women’s health. Register today! shorturl.at/KDQGZ

Gorgeous day for football! New York Giants

New American Thoracic Society (ATS) workshop exploring the links between #osa and #cvd. One thing is clear: OSA is not a single disease entity! Co-chairs Neomi Shah Klar Yaggi Vaishnavi Kundel, MD, MS atsjournals.org/doi/10.1513/An…
Beyond THRILLED to share that our team’s #research proposal to conduct a study on #Menopause-Associated #Insomnia Treatments has been approved for $14.1M in The Patient-Centered Outcomes Research Institute funding! Learn more: pcori.org/research-resul… #CER Susan Redline Kelly Baron, PhD, MPH, DBSM Katie Sharkey MD PhD (she/her) Heather Baer...

nytimes.com/2024/12/19/wel… via @NYTimes Great insights from Oren Cohen featured in the article ‘How to Actually Sleep on an Airplane.’ Practical tips! ✈️ Mount Sinai Department of Medicine ATS Early Career ATS Early Career AASM Foundation