
Adrianne R Bischoff
@arbischoff
Clinical Assistant Professor -Neonatal Hemodynamics Specialist at @uichilldrens @uihealthcare. My opnions are mine, not the opinions of the University of Iowa.
ID: 1648713848348721153
http://www.adriannerahdebischoff.com 19-04-2023 15:43:15
409 Tweet
861 Followers
487 Following









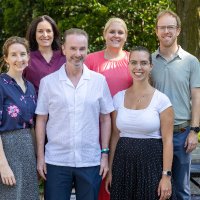
Thankful to have such a great group of motivated physicians at our Observership Experience this week! Learn more: gme.medicine.uiowa.edu/neonatology-he… Rachael Hyland, MD Adrianne R Bischoff Dilara Mat Numra jwrenmdphd

















