
#MondayNightIBD
@mondaynightibd
Created by @DCharabaty •Join us for #IBD #IBDPoll & convo or #Back2Basics MON ~5pmET • #PatientExperience WED • #IBDAlgorithm THUR • Opinions≠med advice 🆓#CME
ID: 1126333259426799616
https://linktr.ee/MondayNightIBD 09-05-2019 03:49:10
7,7K Tweet
9,9K Followers
855 Following

#MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS 70M pancolitis+PSC, on ADAL, o/w healthy 🔦Surv CLN: depressed lesion in sigmoid (📸 👆🏽) 🔬Bx of the lesion: high grade dysplasia. Random bx proximal rectum: indefinite dysplasia, distal rectum: nml What do you recommend? 🔑TPC= total proctocolectomy; IRA= ileorectal anastomosis

Nayantara Coelho #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Great case Nayantara Coelho Looking at the lesion it looks slightly depressed- which always makes me worry there’s already CA even if bx + HGD. how do you describe this lesion- any role for endo resection if a pt is not a surgical candidate? Gursimran Kochhar MD Benjamin Clement, MD

#MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Good point! Lesion is Paris IIc. But second picture shows effaced blood vessels. High risk of adenoca- as in this case. ESD outcomes not well defined in this morphology. Refs in reply

#MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS pubmed.ncbi.nlm.nih.gov/39848273/

#MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS pubmed.ncbi.nlm.nih.gov/40275777/

Nayantara Coelho #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Assuming good sphincter function in a 70yo, would you offer IPAA? Or is this patient at high risk of malignancy in pouch/cuff. How significant is the indefinite dysplasia in proximal rectum in this case? Jordan Axelrad, MD, MPH Dr Jonny Blackwell Dr Feza Remzi Pär Myrelid Shrinivas Bishu

Aline Charabaty, MD, FACG, AGAF #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu IPAA an option here but needs surv. Rectal dysplasia strong risk for iPaa dysplasia pubmed.ncbi.nlm.nih.gov/38422398/

Aline Charabaty, MD, FACG, AGAF Nayantara Coelho #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu If he’s had long-standing disease and he’s starting to have dysplasia, the colon & rectum should come out. Needs really thorough preop risk/benefit discussion “Easy answer” TPC/EI But pt choice- can have IPAA at 70 but ⬆️ complications + pouchitis w/PSC Try for double-stapled🤞

David M. Schwartzberg, MD Aline Charabaty, MD, FACG, AGAF #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu Agree. pubmed.ncbi.nlm.nih.gov/33544128/

Nayantara Coelho Aline Charabaty, MD, FACG, AGAF #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu Agree with IPAA as a reasonable option. Sounds like as a first step we are all in agreement that surgery needs to happen in this very high risk PSC patient.

Nayantara Coelho David M. Schwartzberg, MD #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu How worried do you get about risk of dehydration w ileostomy in a frail vs Fit vs elderly ? Any role for L hemi & colostomy w close endo surveillance ? Stefan Holubar MD MS Adam Faye MD MS Beatriz Gros Paula Sousa Neilanjan Nandi, MD, FACG, AGAF, FCCF, FACP Tauseef Ali MD, FACG AGAF FACP

Aline Charabaty, MD, FACG, AGAF Nayantara Coelho David M. Schwartzberg, MD #MondayNightIBD AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Dr Jonny Blackwell Dr Feza Remzi Shrinivas Bishu Beatriz Gros Paula Sousa Neilanjan Nandi, MD, FACG, AGAF, FCCF, FACP Tauseef Ali MD, FACG AGAF FACP Certainly part of the consideration. Would have to discuss ability to manage the ostomy/output etc - but given concern for future invisible dysplasia (assuming otherwise doing well)- upfront EI (or possibly IPAA) may be preferred

Nayantara Coelho #MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Agree that the depressed + ulcerated nature of the lesion don't make it a good candidate for endoscopic resection. Careful shared decision making is key here. Safest to reduce cancer risk = TPC/EI. If pt adamant against permanent ostomy, consider partial colectomy w close surv

Nayantara Coelho #MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS There are several studies that support consideration of segmental colectomy in carefully selected UC patients. E.g. pubmed.ncbi.nlm.nih.gov/38653494/ In my experience Memorial Sloan Kettering Cancer Center, many patients are pretty emphatic in accepting the risk of metachronous lesions rather than upfront TPC

David Faleck #MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Memorial Sloan Kettering Cancer Center Agree in general. But in an older patient, with rectal disease, segmental is harder. Much easier decision in right sided lesions.

Nayantara Coelho #MondayNightIBD Aline Charabaty, MD, FACG, AGAF AbbVie JanssenUS Takeda Nisha Loganantharaj David Fudman, MD Jordan Axelrad, MD, MPH Tanvi Dhere,MD David M. Schwartzberg, MD Stefan Holubar MD MS Edward Loftus Jami Kinnucan, MD, FACG, AGAF, FCCF Pär Myrelid Adam Faye MD MS Memorial Sloan Kettering Cancer Center Agree, no ideal options here. L-sided/rectal neoplasia does pose additional challenges, but if the rectum is quiescent for years on medical therapy and patient understands the limitations (including need for close surveillance of the indef dysplasia) then it can be considered.

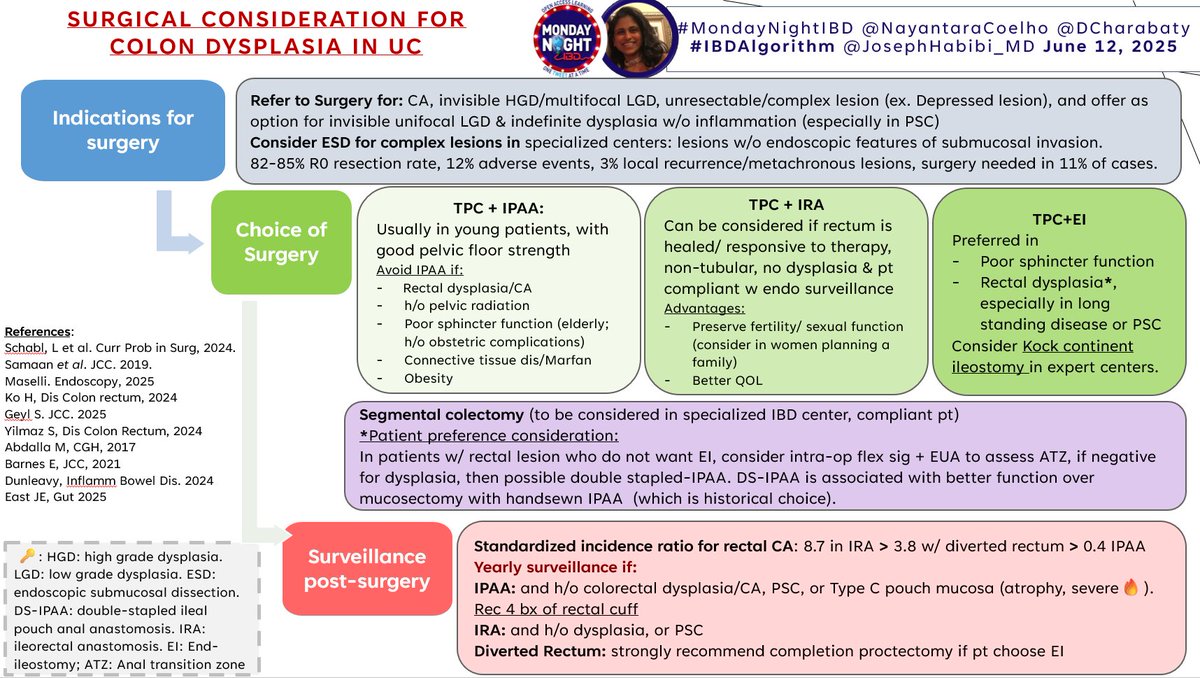
#MondayNightIBD Katie Dunleavy Romy Chamoun, MD Nayantara Coelho Dr Feza Remzi Peter Higgins Gastroenterology Jordan Axelrad, MD, MPH David Fudman, MD Shrinivas Bishu Anjan Dhar Shomron Ben-Horin Edward Loftus American Gastroenterological Association (AGA) Tanvi Dhere,MD Samiksha Pandey, MD, MSc Saqr Alsakarneh, MD, MSc #IBDAlgorithm #MondayNightIBD Aline Charabaty, MD, FACG, AGAF 🎯Surgical Considerations for colon dysplasia in IBD Nayantara Coelho 📡When to refer to surgery vs ESD ✅Nuances of surgical options ✅Post-op surveillance remains key 🎯PostConvo polls🗳️👇(Answers in #IBDAlgo & slides👆)

#MondayNightIBD Katie Dunleavy Romy Chamoun, MD Nayantara Coelho Dr Feza Remzi Peter Higgins Gastroenterology Jordan Axelrad, MD, MPH David Fudman, MD Shrinivas Bishu Anjan Dhar Shomron Ben-Horin Edward Loftus American Gastroenterological Association (AGA) Tanvi Dhere,MD Samiksha Pandey, MD, MSc Saqr Alsakarneh, MD, MSc Aline Charabaty, MD, FACG, AGAF Pär Myrelid Muddasir Ayaz David Faleck Kajali Mishra Sanchu Bhasin David M. Schwartzberg, MD Jana G Hashash, MD, MSc Edward Barnes MD MPH Adam Faye MD MS Anita Afzali MD, MPH, MHCM, FACG, AGAF 1/ #MondayNightIBD #PostConvo #IBDPoll 1️⃣ 🆓#CME👉🏼bit.ly/PrabhuPost 32M with panUC > 8yrs in remission on VDZ. 🔦surveillance CLN: multiple pseudopolyps but no adenomatous lesion to be removed 🔬Random bx: no dysplasia. His father had colon cancer in his late 40’s. 🗓️Per

#MondayNightIBD Katie Dunleavy Romy Chamoun, MD Nayantara Coelho Dr Feza Remzi Peter Higgins Gastroenterology Jordan Axelrad, MD, MPH David Fudman, MD Shrinivas Bishu Anjan Dhar Shomron Ben-Horin Edward Loftus American Gastroenterological Association (AGA) Tanvi Dhere,MD Samiksha Pandey, MD, MSc Saqr Alsakarneh, MD, MSc Aline Charabaty, MD, FACG, AGAF Pär Myrelid Muddasir Ayaz David Faleck Kajali Mishra Sanchu Bhasin David M. Schwartzberg, MD Jana G Hashash, MD, MSc Edward Barnes MD MPH Adam Faye MD MS Anita Afzali MD, MPH, MHCM, FACG, AGAF 2/ #MondayNightIBD #PostConvo #IBDPoll 2️⃣ 🆓#CME👉🏼bit.ly/PrabhuPost In a patient with IBD undergoing surveillance colonoscopy, which dysplasia can be resected by endoscopy (answer in B2B🧵)

